Sep 5, 2024
Where UPMC Enterprises Sees Opportunities for Innovation in Surgical Robotics
By Harrison Lands, MD, MBA, Director, Translational Sciences, UPMC Enterprises
The first time I saw a surgical robot in medical school I was amazed at how artfully the surgeon manipulated the tools to delicately dissect tissues — feathering the foot pedals to seamlessly switch between tools all while keeping the perfect view. I had seen videos of surgical robots being used to peel the skin off grapes but didn’t quite understand their power and precision until I witnessed one in action firsthand.
But I also have experienced the frustrations associated with robots — waiting more than an hour for a procedure to start due to delays in properly setting up and calibrating the machine for a procedure that potentially could have been performed without robotics.
Robots are a great tool when employed correctly, but there’s much innovation to be had in the space. They are expensive, take up significant space in operating rooms, and the patient outcomes achieved with surgical robots don’t always justify their high costs.
As a director on the Translational Sciences team at UPMC Enterprises, I am tasked with evaluating complex opportunities and expanding our reach into medical devices. We have become increasingly interested in medical device opportunities — many of which fall into the exciting and growing category of surgical robotics.
In the following essay, I will lay out the surgical robotic landscape, highlighting the benefit and challenges with these systems, and conclude with where UPMC Enterprises sees the greatest opportunities for innovation.
Surgical robot landscape
Surgical robots are found throughout many hospitals but are primarily used in operating rooms. At UPMC, one of the nation’s largest integrated provider and payer health systems, these robots help with everything from spine procedures to complex abdominal surgeries — with many benefits for patients and physicians.
While many people are likely most familiar with da Vinci surgical robots, those so-called “master-slave” systems are just one of four categories of surgical robotics.
A “master-slave” system: In these systems, a surgeon controls the end effectors at a console. These types of soft tissue robots are most associated with the medical device giant Intuitive Surgical, which pioneered the space of surgical robotics in the 1990s with its da Vinci robot line. To date, Intuitive makes up more than 90% of the surgical robot market by revenue, showing the dominance it has continued to have over this market.
UPMC has dozens of da Vinci systems across its broad hospital network for use in urology, thoracic surgery, colorectal surgery, and gynecological surgery among other surgical specialties.
Recently, Johnson & Johnson announced its Ottava robot, with robotic arms integrated into the operating table, to compete with the da Vinci. There is also Medtronic’s Hugo robot in this category. It will be interesting to see if newer entrants to this space will be able to chip away at Intuitive Surgical’s behemoth share of the market.
Orthopedic robots: The second type of robots are navigational orthopedic robots, such as Stryker’s Mako system. These systems synch with pre-operative CT scans to aid placement of hardware and for making precise bone cuts. These robots position themselves so surgeons can precisely place screws in spine surgeries and guide saws during knee replacements. At UPMC, we have many spine and knee/hip robots in our orthopedic and neurosurgery departments.
Endoluminal robots: An emerging category of surgical robot is the newest of all and therefore much more diverse with the greatest number of startups in recent years. Known collectively as endoluminal robots, these devices navigate the natural orifices of the human body, often employing scopes and tools to aid with minimally invasive diagnosis, screening, and even therapeutic actions.
These types of robots have seen the greatest traction in the respiratory world, with robotic bronchoscopes, such as Intuitive’s Ion and Johnson & Johnson’s Monarch, enabling access to sites within the airway that otherwise would not be reachable with the manual navigation of traditional bronchoscopes. Robotic platforms with similar abilities are also being developed for the gastrointestinal tract. Recently, there has been a push for endovascular robots that hope to revolutionize stroke treatment by enabling remote providers in academic medical centers to operate robots in rural hospitals that do not have expert physicians on staff.
Purpose-built niche robots: The final category I’ll reference is robots that do one thing really well. These robots aid surgeons in performing simpler procedures, such as Iota Motion facilitating cochlear implantation while preserving residual hearing in the process. These robots are typically cheaper and take up a smaller footprint than traditional robots as they are engineered from the ground up to do their specific job.
Benefits of surgical robots
So why has there been so much attention paid to and money spent on surgical robotics? As highlighted in the graphic below, there are many benefits to employing these systems.
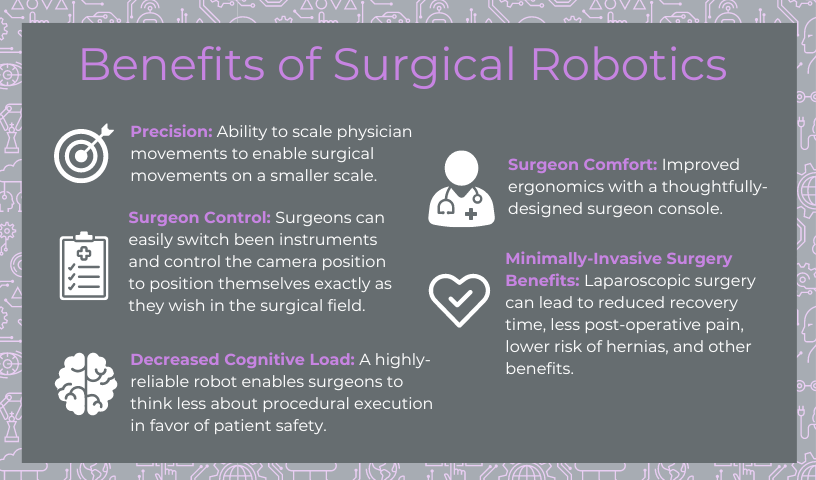
The scaling of larger human movements to smaller robot arm movements enables extreme precision and accuracy that allows surgeons to perform delicate procedures at a micro scale (My earlier reference to robots peeling a grape). The robot also doesn’t face the same fatigue limitations of humans. If you put a tool in a specific position and lock it there with a robot, it won’t move, whereas humans over time will become tired and surgical implements may drift.
“Master-slave” systems have wristed arms which enable dexterity that’s similar to working by hand, but in a minimally invasive way. Surgeons can position tools and robotic cameras into deep holes or around corners in ways that couldn’t be done laparoscopically and would ultimately require larger incisions. Surgeons, at the console, have greater control over all the instruments. Surgeons can switch between robotic arms and move them to the exact position they want — rather than directing a lesser-experienced surgeon to do so. This increased control enables greater consistency in outcomes.
Finally, the ergonomics of sitting at a console cannot be downplayed. Surgeries often last for 10+ hours and standing in uncomfortable positions can take tolls on surgeons’ bodies and potentially limit their ability to operate later in life. Being able to operate for long hours in a way that places less stress on the body is one of the main reasons surgeons love their robots.
Challenges in surgical robot adoption
However, not all is rosy when it comes to surgical robots as their adoption faces many headwinds. Some of those challenges stem from larger macroeconomic pressures within health care to reduce costs. But others are potentially solvable.
Robots are expensive: Some platforms cost more than $2 million dollars to adopt. In addition to the significant upfront costs, there are recurring costs including maintenance contracts and the disposables necessary for each procedure. This problem becomes even more salient with some robots that are hyperspecialized and have limited applications across specialties.
Operating room space is precious: Every square inch in an operating room is valuable. Surgical robots are often large and difficult to move so the surgeon console and robot tower sit either permanently in the operating room or in a hallway nearby. Sometimes this translates into extended time to setup and takedown the robotic equipment in a sterile manner.
But do robots need to take up this much space? Newcomers to the space are developing robots that are smaller, use fewer robotic arms, and are targeted for ambulatory surgery centers. Some examples include the Virtual Incision MIRA, Vicarious Surgical Robotic System, and the Moon Surgical Maestro.
Clear benefit to patients is required. Finally, surgical robots do some amazing things including enabling surgeries not possible in minimally invasive approaches using laparoscopy. However, the clinical outcomes do not always support the need for robotics. Many studies have failed to show any differences in outcomes between robotic and non-robotic methods, calling into question the “raison d’être” or need for surgical robotics.
Conclusions
With those challenges in mind, we believe at UPMC Enterprises that new surgical robotics companies will need to demonstrate the following attributes to be successful:
- They will need to be more affordable to enable less friction in uptake by hospital systems, or be able to support multiple procedures to maximize utilization.
- Cost savings need to be both in the upfront costs and the perpetual disposables down the road.
- Have streamlined and efficient setup and takedown times such that they become easily integrated into operating room workflows and minimize disruptions to surgical procedures.
- Finally, and maybe most importantly, these robots will need to improve patient outcomes to justify their usefulness and support their adoption.
When it comes to the four categories, the level of opportunity varies. While Intuitive Surgical holds a dominant position in the soft tissue robotics category, there may be opportunity for innovative companies to develop technologies that complement the da Vinci or have use cases not currently offered by Intuitive. In orthopedic robots, there would appear to be saturation of the space. Which leaves the emerging space of endoluminal robots. While this niche has yet to be fully embraced there appears to be more opportunity for innovation here. It is important to note that these robot categories are not static as the surgical landscape evolves and new technologies and entrants emerge. We will continue to engage with our clinical colleagues to ensure we stay on top of trends.
The surgical robotics space is exciting and evolving rapidly. I believe many new innovations will be coming to market soon and UPMC Enterprises wants to partner with best-in-class life sciences companies that are targeting areas of high unmet medical need.
Next steps
- If you are developing a surgical robot or know of a medical device company aligned with our interest, please reach out our investment team using the contact us form.
- Learn more about the Translational Sciences team at UPMC Enterprises and how it leverages scientific, clinical, and investment expertise to developing innovative therapies and products.
About the author
Harrison Lands, MD, MBA, is a Director at UPMC Enterprises on the Translational Sciences team. He is responsible for leading diligence efforts on potential investment opportunities. Harrison was a general surgery resident at Dartmouth and, prior to joining UPMC Enterprises, a consultant at Boston Consulting Group helping to advise health care companies.
Harrison completed his dual MD/MBA degree at the University of Virginia. He received his undergraduate degree from Swarthmore College, graduating with High Honors. Harrison was born and raised in Toronto, Canada, and enjoys spending time with his wife and his dog, Moose.