Oct 16, 2024
Unlocking Potential: How AI is Transforming Clinical Trials
In today’s technologically advanced era, the integration of artificial intelligence (AI) and clinical trials has the potential to drive groundbreaking innovations in health care.
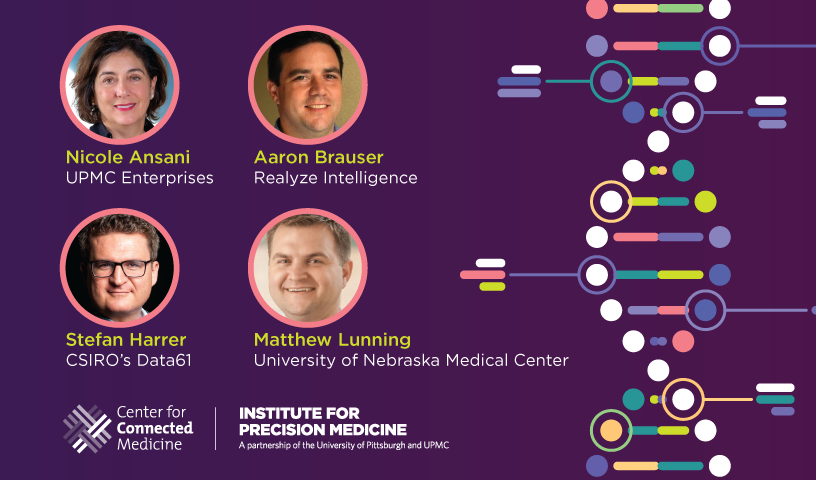
The Center for Connected Medicine (CCM) and the Institute for Precision Medicine (IPM) at UPMC and the University of Pittsburgh explored this topic during a virtual panel discussion titled “Optimizing Clinical Trials at Health Systems: The Opportunity for AI” on Thursday, Oct. 3.
Moderated by Nicole Ansani, PharmD, Senior Vice President of New Development Initiatives at UPMC Enterprises, the event featured the following experts:
- Matthew Lunning, DO, Assistant Vice Chancellor of Clinical Research at the University of Nebraska Medical Center
- Stefan Harrer, PhD, Director of Artificial Intelligence for Science at CSIRO’s Data61
- Aaron Brauser, CEO of Realyze Intelligence
The panel discussed how AI can enhance the efficiency and equity of clinical trials and provided valuable insights on utilizing AI to streamline patient recruitment, enhance trial design, and tackle ethical concerns.
The Promise and Challenges of AI and Clinical Trials
Adrian Lee, PhD, Director of the Institute for Precision Medicine, opened the panel discussion by emphasizing the essential role of clinical trials in assimilating precision medicine into personalized care.
“The goal of this collaboration [with the Institute for Precision Medicine] is to move precision medicine research into personalized care, breaking down the barriers and accelerating our goal of improving patient outcomes,” Dr. Lee said.
He also acknowledged the vast potential of AI and noted the significant challenges the powerful solutions can present. The increasing complexity of precision medicine and clinical trials make recruitment and execution more difficult, thereby slowing progress. Dr. Lee said he is hopeful that challenges can be overcome with AI technology.
The Need for Innovative Methodologies
Laying the foundation for the moderated portion of the panel, Dr. Ansani highlighted a striking statistic, revealing that only 1 in 7 molecules entering Phase 1 trials successfully reach the market, stressing the urgent need for innovative clinical trial methodologies.
As the conversation progressed, the panelists deliberated the current applications of AI, emerging opportunities in pre-clinical research and trial design, and crucial challenges such as data biases, ethical concerns, and the lack of regulatory guidance that complicates AI’s integration into health care.
The discussion concluded with the panelists in unanimous agreement that as clinical trials increase in complexity and cost, AI will be a vital strategy to enhance clinical, operational, and financial efficiencies for clinical trials.
Key Takeaways from the Panel
- Enhancing Patient Recruitment: Nearly 90% of trials fail to meet enrollment timelines, with one-third of Phase 3 trials facing similar issues. AI can streamline patient recruitment by analyzing extensive datasets to identify suitable candidates efficiently. Brauser stated that Realyze Intelligence has improved enrollment rates by over 20% and increased screening efficiency by 20 times, especially in rural areas where finding eligible patients is challenging.
- Improving Trial Design: AI aids in designing effective trials by predicting outcomes and anticipating potential issues. Dr. Harrer discussed using AI-powered digital twins to simulate patient cohorts, which reduces the number of actual patients required and complements real patient data. This approach is especially beneficial for rare diseases with limited patient pools.
- Mitigating Ethical Concerns: The use of AI raises ethical considerations, particularly around patient data privacy and algorithmic biases. Ensuring proper consent for data usage and addressing historical biases are vital for maintaining trust in clinical trials.
- Empowering Patients: AI tools can empower patients by providing information about available trials and their eligibility, leading to increased participation and engagement. Dr. Lunning highlighted that patients are becoming more proactive, often seeking trials online and expecting shared decision-making in their health care. AI can facilitate this process by matching patients with suitable trials and providing relevant information.
- Continuous Monitoring and Adaptation: AI enables ongoing monitoring of trial participants, allowing for real-time adjustments and interventions. Dr. Harrer shared insights on digital disease diaries that use AI to track patients’ daily routines, detect disease episodes, and monitor medication adherence. This can enhance patient compliance with trial protocols and reduce dropout rates, leading to more reliable outcomes.
The Future of AI in Clinical Trials
Integrating AI into clinical trials presents challenges, such as data quality, but the potential benefits are immense. AI can create a more efficient, equitable, and effective clinical trial process, accelerating new treatment developments and advancing personalized medicine. To fully realize AI’s potential, collaboration among health care providers, researchers, and technology developers is essential. Unlocking AI’s capabilities in clinical trials can pave the way for brighter patient outcomes and foster a more equitable health care landscape for all patients.
Next Steps
- Watch the On-Demand Panel Discussion
- Download the Center for Connected Medicine Report: ‘How Health Systems are Navigating the Complexities of AI’